15 - Mental Health Flashcards
What is the difference between low mood and depression?
A low mood can happen when you are having some distressing events happening in your life, often lasts for a few days and then lifts
Depression lasts for several weeks and can often be feeling low for no apparent reason

What are the typical presenting features of depression?
Two core symptoms:
- Persistent low mood, feeling down, depressed and hopeless
- Little pleasure or interest in doing things
Other symptoms:
- Disturbed sleep (decreased or increased).
- Decreased or increased appetite and/or weight.
- Fatigue/loss of energy.
- Agitation or slowing of movements.
- Poor concentration or indecisiveness.
- Feelings of worthlessness or excessive/inappropriate guilt.
- Suicidal thoughts or acts

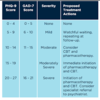
How is depression sorted into a category e.g mild, moderate?
Subthreshold: at least two, but fewer than five symptoms
Mild depression: symptoms in excess of five symptoms and they result in minor functional impairment.
Moderate depression: symptoms or functional impairment are between mild and severe.
Severe depression: most symptoms and they markedly interfere with functioning – with or without psychotic symptoms.
Persistent subthreshold depressive symptoms (dysthymia):
subthreshold symptoms for more days than not for at least 2 years, which is not the consequence of a partially resolved ‘major’ depression

What are some investigations you may do for a patient when diagnosing them with depression?
Rule out other illnesses causing the depression, e.g TFTs, FBCs, dementia, LFTs, U+E’s, ESR, Ca levels
What is the PHQ9 questionnaire and how is the score interpreted?
Score out of 27:
0-4 none
5-9 mild
10-14 moderate
15-19 moderately severe
20-27 severe
5,10,15,20 are all cut off scores

What is the HADS scoring system for depression? (Hospital Anxiety and Depression Scale)
Max score for each subscale is 21
8-10, 11-14, and 15-21 represent cut off points for mild, moderate and severe depression

What is the BDI-II (Beck’s) questionnaire for depression?
21 questions each with a score out of 3
Scores of 14-19, 20-28, and 29-63 can be interpreted as mild, moderate, and severe depression respectively

What are some risk factors for depression?
- Older age
- Recent childbirth
- Stress, or trauma
- Co-existing medical conditions
- Personal or family hx of depression
- Certain medications (e.g., corticosteroids)
- Female

How is the definitive diagnosis of depression made?
- Low mood for most days for two weeks and 4 other symptoms of depression
- FBCs only used to rule out other causes of symptoms like fatigue like thyroid issues, anaemia
How is depression monitored?
- Follow up within the first 2 weeks of prescribing antidepressants to address adverse effects, suicidality, and acceptance of medication taking. Adherence low in depression
- During the 12 week maintenance phase check on patient monthly
- Once symptom remission patients should stay on drug regime for 9-12 months
- Use PHQ9 to monitor symptoms, want a decrease by 50%

What are some complications that can arise when starting a patient on antiepressants?
- SSRIs/SNRIs can cause loss of libido, increased risk of self harm and suicide especially if <25, agitation, unmasking mania if underlying bipolar
- Mirtazapine can cause weight gain
- Antidepressant withdrawal mania
-Antidepressant discontinuation syndrome (when taking for 6 weeks then abruptly stop get symptoms like flu, insomnia, nausea, hyperarousal)

What is the prognosis with depression?
Goals are complete remission. Once remission of symptoms treatment should continue for 9-12 months
.
Third of patients will relapse in a year after stopping treatment and 50% of patients will relapse in a lifetime.
For those who relapse long term antidepressants treatment is advised

How should depression be managed in primary care?
- Manage any suicide risk
- Manage any comorbities and safeguarding concerns e.g psychotic symptoms, eating disorders
- Offer sleep hygiene
- Arrange follow up within 2 weeks
- Subthreshold depression: active monitoring, provide info about the nature and course, follow up in 2 weeks
- Mild to moderate depression/persistent subthreshold: low intensity psychosocial intervention by referral or self referral to IAPT e.g Let’s Talk, group based CBT, avoid routine use of antidepressants unless history of depression or threshold symptoms for at least 2 years
- Moderate or severe: high intensity psychosocial intervention and antidepressants

What is the difference between low intensity and high intensity psychological interventions?
Low intensity: individual guided self help, group based CBT, computerised CBT
High intensity: interpersonal therapy, behavioural activation, couples therapy, individual CBT, counselling and short term psychodynamic psychotherapy

What advice should you give to someone starting antidepressants?
- Explain suicide risk
- Symptoms of anxiety may get worse before they get better
- Explain they need to be used up to 6 months after remission to reduce risk of relapse
- Explain antidepressants can take time to work (6-8 weeks)
- Do not suddenly stop taking them

What antidepressant should you prescribe for someone presenting with depression?

1st Line: SSRI citalopram, fluoxetine, paroxetine, or sertraline. Sertraline has lowest drug interaction and cheapest so first line
2nd Line: different SSRI or Mirtazepine (TCA)
3rd Line: SSRI + Mirtazepine or Venlafaxine (SNRI)
May be offered lithium after lots of other antidepressants tried

What are the side effects for antidepressants?
Side effects should improve in a few weeks

SSRIs and SNRIs: shaky, stomach ache, nausea, loss of appetite, insomnia, headaches, low sex drive, erectile dysfunction, difficulty achieving orgasm, hyponatraemia, suicidal thoughts, risk of diabetes
TCAs: dry mouth, blurred vision, weight gain, constipation, problems passing urine, excessive sweating, palpitations, tachycardia, risk of diabetes
Lithium: dry mouth, metallic taste in mouth, shaking hands, diarrhoea, need to eat salt to prevent lithium toxicity
Which antidepressants should be used/not used when patients are also on the following medications:
- NSAIDs/Aspirin
- Warfarin
- Heparin
- Triptans
- Flecainide
- NSAIDs: do not offer SSRI, offer mirtazapine. If need SSRI give gastroprotection
- Warfarin: do not offer TCA, SSRI, do offer mirtazapine
- Heparin: do not offer SSRI, any alternative will do
- Triptans: do not offer SSRI, offer mirtazapine
- Flecainide: do not offer citalopram as long QT!!! offer sertraline

What is serotonin syndrome?
Often begins a few hours after taking a new drug or increasing the dose of a drug that increases serotonin
Symptoms: confusion, agitation, dilated pupils, nausea, vomiting, see image
If left untreated can lead to seizures, kidney failure, coma and death

What are some places you can signpost patients too with depression?
- IAPT Let’s Talk
- Mind
- Samaritans
- Mental Health Facilitators
- Juniper Lodge (sexual assault)
- Crisis
- Hub of Hope
- Turning point

What are some self help strategies you can advise patients with depression to try?
- Meditation e.g Headspace
- Regular exercise e.g yoga
- Healthy eating
- Self help books and mindfulness
- Sleep hygiene

What should you advise a patient who asks if St John’s Wort will help their depression?
Advise them not to take it as it induces and inhibits CYP450 enzymes so causes lots of other drug interactions
What monitoring needs to be done on antidepressants?
- Suicidal thoughts
- ECG if taking citalopram or escitalopram as may causes long QT and torsades de pointes. Do when palpitations, vertigo, syncope, or seizures develop or before treatment if have cardiac disease
- BP before and whilst taking duloxetine and venlafaxine as can cause HTN
- HypoNa, if at high risk measure every 3 months