14 - T&O Ankle and Foot Flashcards
What is the definition of an ankle fracture?
Fracture of any malleolus (lateral, medial or posterior) with or without disruption to the syndesmosis
Tibial articular surface (plafond) fracture is not an ankle fracture this is a Pilon fracture

What is the ankle syndesmosis?
Fibrous structure consisiting of anterior inferior tibofibular ligament (AITFL) and posterior inferior tibiofibular ligament (PIFL) and interosseous mebrane

How are ankle fractures classified?
- Anatomically: e.g isolated lateral malleolar fracture, bimalleolar fracture, trimalleolar fracture
- Weber Classification (Classifies lateral malleolus fractures)
- Lague Hansen classification

How will an ankle fracture present?
- Ankle pain
- Associated deformity if fracture dislocation (urgent reduction)
- Check for neurovascular compromise and skin integrity for open fracture

What investigations should you do if you suspect an ankle fracture?
- Plain radiography AP and Lateral with ankle dorsiflexed as talus can look translated in mortise when plantarflxed
- If complex use CT scan
- Use Ottawa rules if diagnostic uncertainty

How are ankle fractures managed?
- Immediate reduction under sedation in A+E then put on below knee back slab
- Repeat post reduction neurovascular exam
- Repeat plain film radiography
Conservative
- If non-displaced medial malleolus fracture, Weber A, Weber B without talar shift, those for surgical intervention
- Below knee back slab for a week then bring back for x-ray and full cast
Surgical
- ORIF if displaced bi/trimalleolar, Weber C, Weber B with talar shift, open fractures

What are the complications with ankle fractures?
- Post traumatic arthritis (rare if appropriate reduction and fixation)
- ORIF: surgical site infection, DVT/PE, neurovascular injury, non-union, metalwork prominence

How are ankle sprains produced and how are they managed?
- High ankle sprain: to the syndesmosis
- Low ankle sprain: damage to ATFL and CFL
Usually due to inversion injury. Fingertip tendeness distal to malleoli, swelling and pain
Get plain film radiograph to rule out bony injury then RICE and early mobilisation
How are calcaneal fractures classified and how do they occur?
Most commonly fractured tarsal bone usually due to axial loading (fall from height). Associated with other fractures
Intrarticular (75%)
Articular surface of subtalar joint, further classified by Sanders Classification. Intra need definitive fixation
Extraarticular (25%)
Avulsion fractures, usually calcaneal tuberosity by Achilles tendon

How do calcaneal fractures present?
- Recent trauma
- Pain and tenderness around calcaneal region
- Inability to weight bear
- Swollen and bruised
- Shortened and widened heel
- Varus deformity
- Assess posterior heel skin integrity (any tenting or blanching needs emergency surgical intervention)

What investigations should you do if you suspect a calcaneal fracture?
- Gold standard CT
- Plain film radiograph (AP, lateral, oblique): will show calcaneal shortening, varus tuberosity deformity, decreased Bohler’s angle
Can do MRI

How are calcaneal fractures managed?
Conservative (<2mm displacement or normal Bohler’s angle)
- Cast immobilisation and no weight bearing for 10-12 weeks
Surgical
- Closed reduction with percutaneous pinning if large fracture but minimal displacement
- ORIF otherwise
- Emergency surgical fixation if any skin compromise
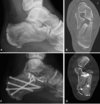
What are some complications with a calcaneal fracture?
Subtalar arthritis that can be treated with analgesia and physio. If unsuccessful with need subtalar arthrodesis

What is the pathophysiology of achilles tendonitis and achilles tendon rupture and what are some risk factors for this?
Repetitive action of tendon results in microtears leading to local inflammtion. Tendon becomes thickened, fibrotic and loses elasticity
Rupture occurs when substantial sudden force (e.g change in direction runnin) applied to tendon when already has tendonitis
Risk factors: unfit individual with sudden increase in exercise, poor footwear choice, male gender, obesity, fluoroquinolone use

How does achilles tendonitis and achilles rupture present?
Tendonitis
Gradual onset of pain and stiffness in posterior ankle that is worse with movement.
Tenderness 2-6cm above insertion site
Rupture
Sudden onset sever pain with audible popping sound. Loss of power of plantarflexion
Do Simmonds Thompson test and feel for palpable step in tendon

How is Achilles tendon rupture investigated and managed?
Ix
Usually clinical but can use US if not sure
Mx
Tendonitis: stop precipitating exercise, NSAIDs, if chronic physiotherapy
Rupture: Analgesia and immobilisation in a plasta full equinus with crutches and no weight bearing. Hold position for 2 weeks then semi-equinus for 4 weeks then neutral for 4 weeks
Delayed presentation (>2 weeks) or rerupture needs surgical fixation with end to end tendon repair

What is the pathophysiology of talar fractures?
Second most commont tarsal bone to fracture, usually in the neck
Usually due to high energy trauma when ankle forced into dorsiflexion causing talus to hit tibial plafond
Talus has retrograde blood supply so fracture causes high risk for AVN

How do talus fractures present and what are some differentials?
- Immediate pain and swelling around ankle
- If dislocation then unable to dorsiflex or plantarflex ankle
- Check if overlying skin is threatened
- Do distal neurovascular status
Differentials: ankle fracture, Pilon fracture
When is skin ‘threatened’? (close to becoming open fracture)
- White
- Non-blanching
- Tethered

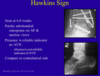
How are talar fractures investigated and classified?
- AP and Lateral plain film radiographs in both dorsi and plantarflexion. Plantar reduces any subluxation present
- CT imaging if complex
- Hawkins Classification used for talar neck fractures to determine risk of AVN

How are talus fractures managed?
Depends on Hawkins class
Type I (Non displaced)
Conservative with plaster and non-weight bearing crutches for three months. Check for evidence of union and AVN in fracture clinic
Type II to IV
Initial closed reduction in A+E, put in cast and repeat radiograph. Then surgical fixation on next available list then period of non-weight bearing

What are some complications of talus fractures?
- AVN (especially in Hawkins II to IV)
- OA secondary to AVN or non-union which may need arthrodesis. Hawkins sign lucency is good predictor of low risk AVN at 6-8 weeks
How are tibial pilon fractures caused?
Plafond fractures are due to high energy axial loads causing the talus to punch up into the distal tbia
Usually from RTA
Usually concurrent injuries like articular impaction, severe comminution, soft tissue injury

How do tibial pilon fractures present?
- History of trauma
- Inability to weight bear and severe ankle pain
- Obvious ankle deformity and swelling
- Fracture blisters in a few hours
Very important to check peripheral pulses and nerves (superficial peroneal, deep peroneal, tibial), comparment syndrome and open fractures

How are tibial pilon fractures classified?
Ruedi and Allgower classification

How do you investigate a suspected tibial pilon fracture?
- Urgent bloods, coagulation and G+S
- If suspect pathological cause do serum calcium and myeloma screen
- Plain film radiograph AP, lateral and mortise view and full view tibia and knee
- CT to plan operation
How is a tibial pilon fracture managed?
- Realignment and then put in below knee back slab
- Repeat neurovascular assessment and plain film radiographs
- Keep limb elevated
- Monitor for compartment syndrome
- Keep NBM with IV fluids in preparation for surgery
- Temporary spanning external fixator then ORIF 1-2 weeks later so soft tissue had time to heal. ORIF best done under traction

What are some complications of tibial pilon fracture surgixal repair?
- Compartment syndrome
- Wound infection or dehiscence
- Delayed or non union
- Post traumatic arthritis
What is a Lisfranc injury?
Severe injuries to lisfranc joint (medial cuneiform and base of second metatarsal) which can be ligamentous or bony
Often missed as subtle radiological features but crucial to diagnose as can lead to ongoing midfoot pain, instability and deformity

How do Lisfranc injuries present?

- After severe torsional or translational forces through plantar flexed foot
- Severe pain in midfoot and difficulty weight bearing
- Swelling and tenderness over mid foot
- Piano key sign
- Plantar bruising
MONITOR FOR COMPARTMENT SYNDROME

How are Lisfranc injuries investigated?

- Plain film radiograph AP, oblique and lateral will show widening of tarsometatarsal joint
- Can take x-rays weight bearing as will increase displacement of Lisfranc joint
- CT for preoperative planning in comminuted fractures

How are Lisfranc injuries classified?
Hardcastle and Myerson Classification

How are Lisfranc injuries managed?
- ATLS protocol to ensure haemodynamic stability
- Closed reduction in A+E with gentle traction to midfoot and then backslab
- Conservative: if non-displaced then cast/air cast boot immobilisation then non-weight bearing mobilisation for 6-12 weeks
- Surgical: temporary external fixation until soft tissue swelling has gone down. then screw fixation or if severely comminuted primary arthrodesis

What are the complications of a Lisfranc Injury?
- Post traumatic arthritis (more common in delayed ORIF and will need midfoot arthrodesis)
- Midfoot compartment syndrome
What are some risk factors for developing hallux valgus?

What is hallux valgus and the pathophysiology of this?
Deformity of the 1st MTPJ where there is medial deviation of the first metatarsal and lateral deviation of the hallux with joint subluxation
More common in woman aged >65, wearing high heels/narrow footwear as holds foot in valgus positon
Metatarsal head escapes intrinsic anatomical control and extrinsic tendons cause metatarsal head to drift mediallly so bone proliferates on medial aspect of head of metatarsal and cartilage remodels

How does hallux valgus present?
- Painful medial prominence aggravated by walking and wearing narrow toes shoes
- Make sure to assess foot non-weight bearing and weight bearing. Check range of movement (active and passive, should be no transverse movement in normal) and crepitus

How is hallux valgus investigated?
- Plain film radiograph to look for lateral deviation and subluxation
- Diagnosed when angle between first metatarsal and first proximal phalanx is greater than 15 degrees

How is hallux valgus managed?
- Sufficient analgesia, adjust footwear, orthosis if flat feet, physiotherapy
- Surgical: metatarsal osteotomy, only done if pain symptoms not just for cosmetic as this procedure can make pain worse

What are some complications of hallux valgus and surgical treatment of this deformity?
Hallux Valgus: AVN, non-union, displacement, reduced ROM
Surgery: wound infection, delayed healing, nerve injury, osteomyelitis
What is the neurovascular supply to the foot?
- Posterior tibial and dorsalis pedis artery (from anterior tibial artery)

What is halux rigidus and how is it treated?
- OA of 1st metatarsophalangeal joint
- ‘Dorsal bunion’
- Stiff toe with reduced ROM
- Analgesia, modify activity, limit movement
- Arthrodesis

What is pes planovalgus?
- Loss of medial longitudinal arch leading to flat foot
- Due to posterior tibialis tendon deformity
- Pain behind medial malleolus
- Usually affects middle aged women

How is adult flat foot treated?
- Insoles and physio
- Last resort surgery. If flexible do reconstruction, if rigid do fusion

What is the gold standard treatment for ankle OA?
Ankle fusion (can replace but not common)

How do you perform a foot and ankle exam in an OSCE?
- GALS
- Look
- Feel
- Move
- Special tests

What is the nerve supply to the foot?

What are the important ligaments in the ankle and what is the importance of the ligament ring?
Ring is like a polo mint, if one area damaged likely there is a nothing point of damage. For example, a fracture in the ankle can be seen on x-ray but ligament damage cannot but fracture indicates ligament damage likely

What is the definition of an ankle fracture?
A fracture of any of the malleoli with or without disruption ot the syndesmosis
What type of fractures does Weber’s classification classify?
Lateral malleolar ankle fractures
What x-ray views would you request in a suspected ankle fracture?
- AP with foot in full dorsiflexion
- Lateral with foot in full dorsiflexion
- Mortise view in neutral
- If posterior malleoli involved get CT
ALWAYS ASK FOR KNEE X-RAY WITH ANKLE FRACTURES AS CAN BE ASSOCIATED INJURY
At what stage in Open Fracture management is the Gustillo-Anderson classification used?
During debridement



