14 - Diabetes Mellitus Flashcards
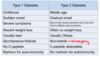
What is type 1 diabetes?
- Absolute insulin deficiency by autoimmune destruction of B-cells
- Mainly in the young
- Rapidly fatal if not treated

What is type 2 diabetes?
- Slow progressive loss of beta cells along with issues of insulin secretion and tissue resistance to insulin
- May be present for long time before diagnosis
- May not need treatment initially

What will blood results from a type 1 diabetic show?
- HLA markers
- Autoantibodies
What is the staging of type 1 diabetes?
- HLA and autoantibodies in blood with no insulin or glucose issues
- Impaired glucose tolerance
- Diabetes
- Insulin dependent

What is the staging of type 2 diabetes?
- Insulin resistance
- Impaired glucose tolerance
- Diabetes

How is type 2 diabetes initially treated?
- Diet
- Tablets
- Insulin
What is diabetes?

What are the two different mechanisms of diabetes?
- Inability to produce insulin due to beta cell failur
and/or
- Insulin production adequate but insulin resistance prevents insulin working effectively

What is the genetic predisposition of type 1 diabetes?
- Genetic marker: HLA DR3 and HLA DR4
- Strong seasonal variation suggesting link with viral trigger
What is the classic picture of type 1 diabetes?
- Lean young person
- Triad of symptoms: polyuria, thirst, weight loss
- Glycosuria
Why do the triad of symptoms occur in type 1 diabetes?
- Polyuria: not all glucose reabsorbe so less water reabsorbed in the nephron
- Thirst: excess water loss in urine
- Weight loss: fat and protein metabolised by tissues because insulin absent
Why does diabetic ketoacidosis occur and how can it be spotted?
- Excess beta oxidation of fats in liver and low insulin/glucagon ratio stimulates ketogenesis
- Large amount of ketones produced and H+
Features: prostration, hyperventilation, nausea, vomiting, dehydration, abdominal pain, fruity breath
Why is it essential to diagnose type 1 diabetes quickly?
Prevent ketoacidosis which is fatal

At diagnosis of type 2 diabetes where are the beta cells at?
- Around 50% functioning and progressively less as time goes on
What are some typical symptoms of type 2 diabetes?
- Triad of symptoms
- Tiredness, weakness, lethargy and weight loss due to inadequate energy utilisation
- Blurring of vision
- Persistent infections, mainly genitalia thrush and feet
- Slow healing

How do you diagnose diabetes?
- Symptoms PLUS
- Random venous plasma glucose conc >11.1 mmol/L
- Fasting plasma glucose conc > 7mmol/L
- Plasma glucose >11.1 mmol/L 2 hours after 75g anhydrous glucose in OGTT
(don’t use finger prick test for diagnosis)

How is type 1 diabetes treated?
- Exogenous insulin subcutaneous several times per day
- Educate patients for times and doses, exercise and diet
- Finger prick BM stick and reader to check sugar levels

When might you change a type 1 diabetic’s insulin dosage?
- Patient suffered trauma or infection need to increase dosage to prevent ketoacidosis
What are some drugs used in the treatment of type 2 diabetes and what else can be used in management of this disease?
- Sulphonylureas: increase insuline release from remaining B cells and reduces insulin resistance
- Metformin: Reduces gluconeogenesis
- Diet and exercise
How can you prevent type 2 diabetes?
- Diet
- Exercise
- Prevent obesity
What is HbA1c?
- Glycated Hb
- Glucose in blood will react with terminal valine of Hb to form glycated Hb
- Healthy 4-6% HbA1c, diabetics 10%

What is the issue with glycation of plasma proteins?
- Glucose reacting with free amino acids to form stable covalent linkages
- Changes net charge and 3D structure of protein so affects function
What are the differences in the urine of type 1 and type 2 diabetics?
Type 2 have no ketones in urine
What are some macrovascular complications of diabetes?
- Increased risk of stroke
- Increased risk of MI
- Poor circulation to peripheries