1.2 - Hypokalemia & Hyperkalemia Flashcards
(12 cards)
What is hypokalemia?
- Serum potassium less than 3.5 mEq/L
- Common clinical problem, cause can often be determined by obtaining a thorough history from the patient
- Serum levels may fall due to body loss or because of cellular uptake from extracellular fluids

What are the 7 common causes of hypokalemia?
1. Renal potassium loss – best measured by a 24 hour urine collection but can be assessed with a spot or random urine. 24 hour urine collection may not be practical if the hypokalemia is severe and potassium replacement therapy is needed emergently.
- Diuretics – Loop (Lasix) and osmotic (mannitol)
2. Mineralocorticoid excess
- Primary hyperaldosteronism of adrenal disease
- Secondary aldosterone excess in hypovolemic states
- Secondary aldosterone excess in renal vascular hypertension
- Renin secreting tumor
- Cushing’s syndrome or adrenal hyperplasia
- High dose prednisone, fludrocortisone, authentic licorice ingestion (exogenous mineralocorticoid effect)
3. Renal tubular disorders – Renal tubular acidosis (RTA), Types I and II, Bartter’s, Gitelman’s or Liddle’s Syndrome
4. Hypomagnesemia
- Nonrenal potassium loss
- Emesis and NG suction
- Diarrhea especially laxative abuse and secretory diarrhea
6. Potassium uptake into cells
- Insulin therapy – common in DKA
- Catecholamine excess – epinephrine or albuterol (beta adrenergic) therapy
- Metabolic diseases: Familial periodic paralysis, thyrotoxic paralysis
7. Inadequate dietary potassium intake (rare)
- Occurs in up to 20% of hospitalized patients and in 10-40% of outpatients who are taking diuretics
What are the subjective and objective findings of a patient with hypokalemia?
- Muscle cramps and tenderness can occur with weakness. Leg weakness may ascent upward to the diaphragm causing paralysis if the hypokalemia is extreme
- Paralytic ileus, abdominal distension, N/V
- Palpitations (varied). High risk with digoxin treatment
- Polyuria and polydipsia. There is an inability to concentrate urine in chronic hypokalemia
- PE will show tender to palpation due to muscle cramps
- Atrial and/or ventricular ectopy can be seen on EKG

What are the laboratory/diagnostic findings of hypokalemia?
Diagnostic approach should include an assessment of urinary potassium excretion and assessment of the acid-base balance
- Serum potassium is less than 3.5 mEq/L
- EKG: T wave flattening, appearance of U waves and possible arrhythmias
-
Urinary K excretion should be assessed.
- If it is greater than 25 mEq/L/24 hr, there is renal potassium wasting
- If it is less than 25 mEq/L/24hr,there is non-renal potassium wasting
- Increased sodium bicarb (HCO3) suggests mineral corticoid excess
- Serum magnesium can be decreased in up to 40% of the patients seen with hypokalemia

How do you replace potassium in patients with hypokalemia?
Review the meds closely, discontinue those that enhance potassium excretion
- Patients with cardiac arrhythmias, especially those on digoxin therapy, those with encephalopathy or those than cannot take oral potassium, use IV KCL, KPO4 and potassium acetate.
- Max solution concentration to avoid vein irritation: 40mEq/L solution in PIV, 60mEq/L for CL. Administer no faster than 10-20 mEq/hr and continuously monitor on EKG
- Oral potassium replacement is most effective with KCL if used.
- If the patient has an acute potassium loss, give 40-60 mEq PO x 1, check K in 4 hr. Can repeat PRN with serial K measurements. If the patient has chronic hypokalemia, give 10-40 mEq/d in 1-2 divided doses
- Can use KCl extended tabs (K-Dur, Micro-K Extencaps)
- Can utilize potassium sparing diuretics in combination with other diuretics to decrease potassium loss
- Spironolactone (Aldactone) 25-100 mg PO daily
- Amiloride (Midamor) 5 mg PO daily
- Epleronone (Inspra) 25-50 mg PO daily
- Encourage intake of high potassium foods to include nuts, dried fruits, tomatoes, potatoes, bananas, oranges

What is hyperkalemia?
- Serum potassium greater than 5.5 mEq/L
- May rise from decreased renal excretion, decreased cellular uptake or increased cellular release of potassium
What are the 7 common causes of hyperkalemia?
1. Decreased renal function occurs when there is:
- Either acute or chronic renal failure
- Decreased aldosterone synthesis seen in adrenal insufficiency or heparin therapy
- Decreased renal aldosterone effect seen in potassium-sparing diuretics and certain renal diseases (diabetic, obstructive or sickle cell nephropathies)
2. Renin-angiotensin system disruption
- Hyporeninemia-hypoaldosteronism most commonly from early diabetic neuropathy
- ACE inhibitor therapy, ARB therapy or the combination of the two
- NSAID therapy
- Cyclosporine therapy
3. Decreased cell uptake/increased cell release
- Insulin deficiency
- Cellular disruption seen in intravascular hemolysis, rhabdo or tumor lysis syndrome after chemotherapy
4. Pseudohyperkalemia occurs in venipuncture only
- Hemolysis from small needle or excess venous occlusion
- Thrombocytosis, platelet count greater than 5000,000/mm2
- Leukocytosis, WBC count greater than 100,000/mm2
5. Metabolic Acidosis-usually hyperchloremic type
6. Digitalis toxicity
7. Increased intake both oral and intravenous

What are the subjective and objective findings of a patient with hyperkalemia?
- Subjective findings include muscle weakness to paralysis
- The symptoms of the underlying disorder that cause the rise in potassium can dominate the patients symptoms
- Physical findings on exam can include both weakness and underlying cause

What are the laboratory/diagnostic findings of a patient with hyperkalemia?
- Serum potassium greater than 5.5 mEq/L
- On the EKG there will be progression of peaked T waves, a widened QRS complex, the disappearance of a P wave, the fusion of QRS and T wave to form a sine wave
- If there is renal failure as cause of hyperkalemia, expect the BUN and serum creatinine to be elevated
- Paired serum renin and aldosterone levels will identify primary or secondary hypoaldosteronism

How do you initiate the medical management of a patient with hyperkalemia?
The urgency and level of intervention is based on the EKG changes
- In all cases of hyperkalemia, repeat the serum potassium for accuracy
- Limit all sources of potassium intake
- Discontinue all drugs that limit the potassium excretion
-
Obtain an EKG
- Normal EKG – give Furosemide 40-80 mg IV to increase excretion
- Sodium polystyrene resis (Kalexalate) 15-45 grams with an osmotic cathartic (sorbital or lactulose) can be given
- Hemodialysis or peritoneal dialysis to remove potassium if renal failure is present
- Abnormal EKG – patient should remain on a monitor until the EKG normalizes.
How do you manage a patient with hyperkalemia with absent P waves, widening QRS complexes or sine waves?
- Calcium gluconate (10%): give 1 gm over 1-2 minutes to antagonize the hyperkalemic effect. This should have immediate onset but can repeat in 3-5 minutes if EKG has nor normalized. This therapy does not lower the potassium, it’s effect can last for minutes only
- Calcium chloride may also be used but need to be careful to avoid calcium toxicity (3 x more calcium present per 10 mls)
- Regular Insulin (10 units) can be given over 2-5 minutes to increase the cellular potassium uptake. Add glucose (D 50%) 25-50 grams if patient is euglycemic. It will have an effect in 15-30 minutes, lasts for 30-60 minutes. It dose not lower serum potassium
- Albuterol (10-20 mg) via inhalation over 10 minutes will help increase cellular potassium uptake, effect seen in 15-20 minutes
- Sodium bicarbonate (50 mEq) IV can be given over 1-2 minutes if the patient is acidotic. If used repeatedly in the patient, it can cause dangerous hypernatremia. Does not lower serum potassium, effect lasts for 2-6 hours.
- Dialysis to remove potassium
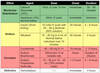
How do you manage a patient with hyperkalemia with only peaked T waves?
- Insulin/glucose or albuterol to increase cellular potassium uptake
- Diuretics, dialysis to remove potassium


