10.03 Muscle, Fuels and Fatigue Flashcards
What are the major functions of skeletal muscle on the whole body level?
- It can comprise up to 40% of total body mass
- Loss of muscle mass in ageing and cancer cachexia is a major cause of death
- Active generation of forces required for power, movement and posture
- It is a major site for deposition of glucose and fatty acids
- Once muscles have optimised their own stores of glucose, remainder in plasma is deposited in fat and taken up by the liver
Characteristics of skeletal muscle are important in detemining metabolic health
What is the evidence to support that contraction (use) of skeletal muscle has important systemic consequences?
Release of myokines from contracting skeletal muscle (IL-6 is a major example) that are able to alter fat, liver, brain and other organ functions
Desribe the relationship between type I muscle fibre composition and fat composition of the body
The more type 1 fibres present, the less fat is present. This is thought to be due to their greater capacity to oxidise fat and use it as a fuel

Describe mitochondrial concentration in skeletal muscle in relation to glucose disposal in the muscles
The higher the mitochondrial mass in muscle, the more glucose is able to be deposited into the muscle (increased ability to utilise energy - oxidative capacity is increased)

What is the evidence to support the idea that muscle is an endocrine organ?
It is believed that the myokines and other important products released from exercised skeletal muscle is important.
Plasma transported from exercise trained mice to non-exercise mice confers an exercise phenotype to these mice
What are the human muscle fibre types?
Type I fibers are also known as slow twitch fibers produce repeated low-level contractions by producing large amounts of ATP through an aerobic metabolic cycle.
Type IIa fibers are also sometimes known as fast oxidative fibres and manufacture and split ATP at a fast rate by utilising both aerobic and anaerobic metabolism and so produce fast, strong muscle contractions, although they are more prone to fatigue than type I fibers.
Type IIx - fast glycolytic fibers produce ATP at a slow rate by anaerobic metabolism and break it down very quicky. This results in short, fast bursts of power and rapid fatigue.
How are the different fibre types seen in immunohistochemistry?
It depends on the pre-incubation method.
Myosin ATPase staining in sections. Type I fibres stain dark after acidic and Type II stain dark after alkaline due to differential acid/alkaline solubility.

How is immunoblotting used to determine muscle fibre types and levels?
The Type 1 fibres have myosin heavy chain 1 while type 2 fibres have myosin heavy chain II.
The troponin C levels is also different between the two muscles

Describe the properties of Type I muscle fibres in terms of the following:

- Low Force
- Slow Twitch
- Low fatigue
- Most abundant
- High mitochondria
- High vascularisation

Describe the properties of Type IIa muscle fibres in terms of the following:

- The fast phenotype
- Second most abundant
- Highest fibre diameter area

Describe the properties of Type IIx muscle fibres in terms of the following:

- Least abundant
- These are the “explosive fibres - high power” seen in high amounts in sprinters

“Speed is born while Endurance is Made”
What is meant by this statement?
They type IIa fast phenotype can be trained to become more fatigue resistant which is what is required for endurance activities.
However the type IIx fibres required for sprinting and speed (high power, short duration events) is very difficult to “make” and train these fibres (born with them)
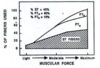
Describe Heddeman’s Size principle of muscle recruitement
Muscle fibres are progressively recruited in relation to the force of contraction.
- Type I fibres first
- Type IIa next
- Type IIx last
This is dependent on both the intensity and duration of force production
What is the composition of muscle fibre types in the 2 major types of athletes and normal untrained people?
- Untrained people have about 50/50 twitch fibre ratios
- Sprinters have low slow twitch and high fast twitch
- Distance runners have high slow twitch and low fast twitch
- Some evidence fast twitch a fibres can become more resistance to fatigue (superfibres)

Describe the distribution of the muscles for different athelete types.
Relate this to the genetics vs. training debate
Extremes (runners) had more slow twich in leg and kayakers more in arm than legs likely due to training But the genetics impact (positve reinforcement) that they were better at one than the other is liekly due to genetics














