#1 Flashcards
What is the most common site of shaft fracture of humerus?
Surgical Neck
What is visible on film, radiographic joint space, or anatomic joint space?
Radiographic Joint space
Does the certified radiology technologist have any liability for diagnostic interpretation? - What reliability do they carry?
no - Carry liability for production of any technical component
Who carries the liability for diagnostic interpretation when providing that service?
General Practitioner
What is the primary responsibility of the radiologist?
Image Interpretation (highest level of service)
Who had the greatest and least % of correct films read in regards to the list in class?
Chiropractic Radiologist = 71.9% Medical Student = 5.74%
If a general practitioner uses a radiologist and gets a report, who has the liability?
Radiologist
Human skeleton has how many bones?
206
Axial skeleton =
74 bones
Appendicular Skeleton =
126 Bones
Chiropractic students had what % of results when correctly identifying pathology?
20.45%
90% of bone metastisis is where?
The Axial Skeleton
Ectodermally derived malignant tumors are…?
Carcinoma
What are the precursors of all structures and organs?
Mesoderm
Malignant tumors that are mesodermal are?
Sarcoma
What is the primary center for ossification?
Diaphysis
What is the secondary ossification center?
Metaphysis
What is a separate structure in kids, but not in adults?
Epiphysis
Aka, “growth plate”
Physis
What part of the bone is a protuberance and functions as an attachment site?
Apophysis
What is the point where tendon/ligament attaches to bone?
Ethesis
What are the only tubular bones to have 1 ossification center?
- Metatarsals (distal)
- Metacarpals (distal)
- Phalanges (proximal)
Describe the cortex…
- Major storehouse of CALCIUM
- Major STRENGTH area of bone
- DENSITY & THICKNESS
Thickness of the cortex is _______ proportional to the diameter of the bone?
INVERSELY
* Cortex is thickest at the narrowest, or center of diaphysis

What is the bone described as when the cortex begins to thin?
Osteopenic

Red and Yellow bone marrow reside where?
Medullary cavity

What are the main sites for Red Bone Marrow in adults?
- Sternum
- Facial Bones
- Ribs

Bone is the __#____ location for metastatic spread?
3
Metastatic cancer spreads to what top 3 regions?
- LUNG
- Brain/Liver
- BONE

Over 2/3 of bone metastisis in women come from?
BREASTS
Who is more likely to have bone cancer?
Adults or Children
CHILDREN
- This is due to the amount of RBM (greater % in kids vs. adults)
What type of bone has marrow in it, and is known as “spongy bone?”
Trabecular

Can you see periosteum on radiograph?
NO
The periosteum has 2 layers, what are they, and what do they do?
OUTER LAYER: Fibrous (insertion layer for tendons & ligaments)
INNER LAYER: Cambium - Labile (Physiologically active)
- Important indicator of BONE DISEASE
How many layers thick is the endosteum?
1
What is at the corticomedullary Junction?
Endosteum

What is significant in adults in regard to the endosteum?
Atrophies a lot in adults
What part of the bone has the function of osteoblastic/clastic function?
ENDOSTEUM
What is “Direct ossification,” and a conversion of mesenchymal tissue into bone without a cartilagenous precursor?
Intramembranous Ossification

Longitudinal bone growth comes from where?
Physis
What is the precursor to appositional bone growth (growth in diameter)?
Intramembraneous Ossification WITHOUT a cartilagenous precursor
Describe Endochondral Ossification with Cartilage
Longitudinal Bone growth**
Mesenchymal cells differentiate into cartilage (later replaced with bone); PHYSIS
What is the MAIN difference between Intramembraneous Ossification and Endochondral Ossification?
- Intramembraneous is mesenchymal tissue into bone
- Endochondral is mesenchymal —> Differentiated cell —–> BONE

What are the 2 major way we grow bone?
- PERIOSTEAL: Blastic/Productive
- ENDOSTEAL: Clastic/Destructive
What is “endochondral bone growth” associated with?
Physis
Physis =
HYPERTROPHIC ZONE & METAPHYSIS****
As the cells move down from the resting layer to the proliferating zone, what happens?
They get larger due to more oxygen availability
**Once they reach the zone degeneration zone they began to die (Lack of OXYGEN)

The reserve/resting zone has what type of blood supply?
Excellent
- Will start growing & make more “blue stuff” = Extra Cartilage Matrix
- As they grow and get larger = Proliferating Layer

The Maturation & Degenerative Zone =
Columnar Layer
Where do cells start to line up in vertical columns?
Maturation Zone
- No blood vessels (avascular)
- Lack of O2
- Cells die
- Need them to die to utilize cells surface area
What are the key features of the primary spongiosa?
- Deminished thickness of mineralized matrix
- Once it’s gone, becomes secondary spongiosa
- CLOSED cappilary loops
- Vasculature - Bring calcium & Phosphorus in Blood (hydroxyapatite)
- Oozes into matrix and mineralizes
How does bone grow occur?
- Bone growth upward meets higher zones –> End of Growth
Rate is influenced genetically, hormonally, and nutritionally
In a pediatric patient, the metaphysis _____ ?
Consists of primary and secondary spongiosa
Cell zone of provisional calcification =
ZONE OF PROVISIONAL MINERALIZATION
- Takes calcium and phosphorus to produce this layer

What allows bone to grow transversely?
Periochondral/Fibrous ring of La Croix
* Supports & at outter peripheral rim of physis

What does the ossification Groove of Ranvier do?
Support and at the outer peripheral rim of physis - Provides cells for growth in width/diameter
What is the physis function?
Endochondral ossification largely avascular, longitudinal bone growth
What do osteoblasts produce?
Osteoids, which are then mineralized to give it rigidity by interacting calcium phosphate appetite

What is the whole point of old cells dying?
We need the SURFACE AREA that it was taking up
** The whole point is to build the matrix (scaffold) and to die for new cells to take its place
Achondroplasia
Genetic mutation (midgets)
- Literally means, “No cartilage growth”

What is categorized as slow endochondral bone formation, and affects (extremity growth)?
Achondroplasia
“hypo” - actually
What is termed as, “greater shortening proximally of (Humerus & Femur)?
Rhizomelia

Where would Someone with Achondroplasia have a great level of stenosis?
L5
- Due to: DJD, or buckling of ligamentum flava
Is appositional growth affected in achondroplasia?
NO
Hydrocephalus may result from what disease?
- Achondroplasia*
- This RESTRICTS the Foramen Magnum

Periosteal bone will have what type of growth in Achondroplasia?
NORMAL
What type of bone growth does Achondroplasia slow down?
Enchondral bone formation (length), but doesn’t impact Periosteal bone growth (Width) and ONLY in APPENDICULAR SKELETON, not axial
* Bones appear FAT
Define ; Tubulation
Formation of tubular bone
Why does the lumbar spine possibly lead to central canal stenosis in achondroplasia?
Pedicles are not long enough

3 most common signs of Achondroplasia:
- L5 has the worst pedicle stenosis
- Horizontal Sacrum is common
- Increased Lordosis
Marfan’s Syndrome
Accelerates rate of longitudinal bone growth

What disease creates bones to look “overtubulated”
Marfan’s

What does Arachondactyly mean?
What disease is associated with it?
Long skinny fingers/toes
- Marfan’s
What type of problems will people with Marfan’s sydrome suffer with?
**Dissecting Aneurysm (Exsanguination)*
- Weaken medial layer, weakens intima, lots of blood goes on mediastinum
kills 1/3
- Occular Issues
Gigantism accelerates what?
BOTH endochondral and periosteal bone formation
(PROPORTIONAL GROWTH)
What is a common problem with Gigantism?
Pituitary tumor (adenoma) making too much HGH
- As adults, the periosteal can still grow so bones get THICKER, but not longer
- Joint cartilage also proliferates (Secondary DJD)
Osteopetrosis
GENETIC
- Alber-Schomberg’s Disease
- Marble Bone
- Chalk Bone

What are people with osteopetrosis prone to?
Anemia: Medullary cavity filled w/ Mineralized matrix. Hematopoetic tissue crowded out
Fracture: Bones become sclerotic, but BRITTLE, decreased blastic activity

What is impacted by osteopetrosis?
Transition from primary to secondary spongiosa (problem converting from primary –> secondary)
What is osteosclerosis defined as?
Increasing bone density

Osteopetrosis makes bone ____ ?
Really sclerotic
What does Osteopetrosis Tarda result in?
Mild form can be turned on, and then off genetically (stop and go process)
_*Erlenmeyer Flask Deformity_

What does the appearance of Osteopetrosis create?
Bone in bone appearance (stop and go sequence)
- Cortex of bone has mostly taken over the bone’s ability to function (becomes anemic)
- Osteoclast are unable to resorb bone and therefore primitive calcified cartilage is ALL OVER

Osteopetrosis Congenita is what type of form?
HYPERACTIVE, and happens all over
- Can’t grow enough marrow to keep up

What is the problem with Rickets/Pediatric Osteomalacia?
Deficiency of Calcium, Vit D, or Phosphorus
- One of the MAIN osteopenic Bone diseases

What is the area of bone that is affected by Rickets/Pediatric Osteomalacia?
Zone of Provisional Mineralization (ZPM) is the area in dispute
- Can’t mineralize matrix (osteocytes) = No “scaffold” = STOPS LONGITUDINAL GROWTH
What does Ricket’s present?
- Bowing* deformity
- Bone is soft
- Doesn’t have enough calcium or phosphorus

Long term rickets =
Dwarfism Disorder
What is the weakest layer of growth plate?
Columnar Zone because cells are big, there’s lots of space, getting ready to die, and they’re lined up in a column

What area of bone would kids be vulnerable to side loading?
Columnar Zone (Marginal & Degenerative)
- TRAUMA
Resting/ Reserve layer vulnerable to AXIAL load injuries (compression)
- Once crushed, bone growth PERMANENTLY stops
What is the least and most common Salter Harris Fracture type?
MOST COMMON: Type 2
- Through physis and apophysis
LEAST COMMON: Type 5
- growth plate crushed

Where does the type 1 Salter Harris Fracture usually occur?
<u><strong>Proximal Femur</strong></u>

- Separates epiphysis from metaphysis through the COLUMNAR LAYER
What is common with Salter Harris Fracture (Type 1)?
Slipped Capital Femoral Epiphysis (SCFE)
- Common injury to HIP of children
What are the details of Salter Harris Fracture type 2?
**** MOST COMMON *****
- Thurston-Hollan Fragment
- Side loaded injury
- MOST COMMON SITES: Distal Radius & Tibia, Fibula Ulna

Salter Harris Type 3 fracture:
Creates a separate epiphyseal piece
(side load trauma)
** Happens with VERTICAL impact

Type 4 Salter Harris Fracture:
Straight Vertical Trauma
- Combined 2 or 3
- MOST COMMON SITE: Fracture through tibia (lateral epicondyle most common in children <10)
- Kid jumps out of Tree

Type 5 Salter Harris Fracture:
Crushes the PHYSIS (extreme pain)
**** Can prematurely STOP longitudinal bone growth if damage to the resting/reserve layer
- Very UNCOMMON, and if it happens, child needs to be followed for 1-2 years to monitor progress (premature fuses)

What is the weakest and most vulnerable layer to fracture in bone?
Columnar (maturation & degeneration)

What layer (if damaged) causes growth to stop?
Resting and Reserve Layer

Main points of Cortical bone anatomy:
- Cortex is DENSE, STRONG, THICK, POREOUS, and made up of cylindrical bone units
- Haversion systems/osteons containing a central neurovascular bundle and interconnected with Volkmann Canals as well as interstitial lamellar bone

What does each osteon have?
Concentric lamellae of bone (holds everything together) with collagen fibers and hydroxyapatite crystals having a unique orientation in each layer (or ring)

What is contained within each lamellar layer?
Osteocytes (mature bone cells) each in its own lacuna, which are interconnected and to the central canal by CANALICULI

How do corticol and trabecular bone differ?
By POROSITY ONLY
Corticol is dense, and trabecular is porous (same type of bone other than that)
What is the main funciton of Periosteum?
_MAKING NEW BONE****_
Is the periosteum pain sensitive?
yes
What builds bone in children?
Subperiosteal Outer Circumferential Lamellae
Are the periosteum or endosteum ever seen radiographically?
oh hell NO
Describe the Periosteum….
a 2 cell layer thick, very vascular and pain potential membrane
What is the outer fibrous layer of the periosteum used for?
Insertion of ligaments and tendons by way of Sharpey Fibers (enthuses) and
Inner cambium layer with OSTEOBLASTIC and osteoclastic potential

How does periosteum grow?
Via Intramembraneous Ossification (found on external cortical surface)
* Increases in thickness as we get older
The endosteum has what type of properties?
A single layer at trabecular and INNER CORTICAL MARGINS, also have both properties
- Predominantly found on the internal cortical surface
- Has clastic and blastic properties
What is the Dominant job of the Endosteum? **
OSTEOCLASTIC***
Eat away at cortex on inside as periosteum expands externally
(They CANNOT work at the same rate)
- _THE ENDOSTEUM HEALS FRACTURES ***_
Endosteum vs Periosteum (work rate):
Endosteal layer is slightly slower, so bones are not the same width as when they’re born. A lot of the endosteum disappears in the adult. Function of both is in balance, but the activity FAVORS the periosteum in IMMATURE skeleton
What happens in the first year of life in regards to bone vascularity?
Epiphyseal and Metaphyseal vessels separate after first year, and some anastamose in infants
* After the first year, physis is a vascular barrier
Metaphysis is _________ area in pediatrics?
*MOST RICHLY VASCULARIZED*****

Infant, Child, and Adult Vascularity (picture & explanation):
- Infant Vascularity (A): Rich metaphysis vascularity, no connection to epiphysis
- Child Vasculartiy (B): Rich metaphysis vascularity connects with and helps epiphysis
- Adult Vascularity (C): Epiphysis and metaphysis connect again after growth plate is closed

Cortex has what type of vascularity?
Unique DUAL from medullary and periosteal vessels
What happens during a bone infection?
All the exudate (pus) takes up space where marrow could be, this will compress blood vessels causing some bone death, causing cut off of medullary supply from cortex. Once it seeps through to the cortex, this will push the periosteum from the bone. This will then rip and tear periosteal blood vessels, thus cutting blood supply and killing the bone.
What is the process of Infection in children?
Exudate (pus) in bone compresses the blood vessels and causes PARTIAL bone death. Medullary blood supply is cut off from the cortex, and it seeps through the cortex, the periosteum is then pushed away from the cortex. Periosteal blood vessels tear, and blood supply is cut off = BONE DEATH
Mylitis =
Only Marrow Infection
Osteomylitis highlights =
- Blood born infection bone and marrow
- Typically spreads from one site to another to the bone
- Most likely to end up in the METAPHYSIS due to the large amount of vascularization
- Infections destroy by pressure or lytic reactions
- In a 5 month old, it can cross from Metaphysis to the Epiphysis

What destroys a joint very fast?
INFECTION (2-3 weeks)

Describe “Thomas Smith Arthritis”
Osteomyelitis
- Goes straight from Metaphysis –> Joint capsule (avoids physis)

How does the cortex have vascularity?
From periosteum vessels through channels, and from nutrient vessels
Define Septic Arthritis
6 month old with infection in metaphysis –> destroys epiphysis up to subchondral bone –> eats through cartilage into joint –> now child has SEPTIC ARTHRITIS (acute osteomylitis in infants)
** Destroys joint in child in weeks what it takes 25 years to happen in adults

Where is the most common site for infection in adults?
Metaphysis (most vascularity is there)
** after 2 years old, there’s no vessels in epiphysis

Acute osteomyelitis is common where in infants?
Nutrient metaphyseal capillaries perforate the epiphyseal growth plate, particulary in the hip, shoulder, and knee
When will infection spread in infants?
Within the 1st year, it is going to spread into the epiphysis from the metaphysis
** Most likely happen in the metaphysis
- Staph (pus forming) and tubercle bacillis (TB) cause most bone infection
What causes most bone infection?
Staph (pus forming) and tubercle bacillis (TB) cause most bone infection
What are the patterns of bone destruction?
Radioluscency
- Periosteal Reactions
- Trabecular Bone changes
- Shape Changes
- Bone Density Alterations
- Soft Tissues
What are the bone lesions?
- OSTEOLYTIC: Destroyed, radioluscent (osteoclastic activity), bone being taken away or being replaced with cancer
- OSTEOBLASTIC: Pathological Process, osteosclerotic (bright white) = more bone produced
-
COMBINATION/MIXED: Combined radioluscent and osteosclerotic. Have both clastic and blastic activity
- Example, Avascular necrosis, mixed metastisis, Pagets

WHat is pictured?

Avascular Necrosis
Ultimately, bones change ____ ?
Shape, Density, or BOTH
What are the main destroyers of bone?
Infection and Tumor
WHat is pictured? Describe it

Bone and mesoderm derived tumor
OSTEOSARCOMA
Primary bone malignancies are _____ ?
Sarcoma

For plain film radiology, must lose minimum of _____ of bone to see actual bone loss ?
30% ***
Describe a “Geographic Lesion”
Area lesion/ Takes up space
- ONE hole
- Benign
- SLOW growing
- Zone of transition is most important

Permeative is the _____ ?
Most aggressive lesion (many holes)

Authors vary on lower limit of size, but a general consensus of ____ seems to be a good standard size for Geographic lesions
larger than 1 cm
Less than 1 cm =
punched out
What is the most important indicator in describing a geographic bone lesion?
Margin (zone of transition)
“edge” of lesion

How are geographic lesions defined?
Subdivided in accordance to their margin:
- 1A
- 1B
- 1C

Describe 1A Geographic Lesion:
Well defined with sclerosis in margin (least aggressive)
- Short transitional zone
- Has a thin rim of bone (looks white) around margin (sometimes thin rim, sometimes thick rim)

Describe 1B Geographic lesion:
Slowest growing of sclerotic lesions. Well-defined, but NO SCLEROSIS in margin
- Short transitional Change

Describe 1C bone lesion:
Geographic destruction with ill-defined margin. Wider or Longer transitional zone (MOST AGGRESSIVE)
** Less distinct where change happens

What does the border or lesion margin indicate?
The general GROWTH RATE
Slow growing benign =
Well defined and a narrow zone of transition often with thin or thick reactive osteosclerosis at the margin 1A
More Agressive Lesions =
Tend to have fainter borders and somewhat wider transitional zone at the margin, may still be benign but more aggressive
* Eg. OSTEOMYELITIS

What bone lesion is OFTEN MALIGNANT?
1C (zone of transition is hard to define)
* This is a great indicator for aggressiveness
Identify

Margin 1 A on top and 1B on the bottom

Geographic lesions may also have little compartments, this would be known as?
Soap Bubble Lesion

When examining the X ray, what are the most important factors?
- AGE
- LOCATION
- APPEARANCE
- SYMPTOMS
ALAS***
Geographic lesions may be what in regards to location?
Centric or Eccentric
Expanison lesions:
Giant cell tumor, may be expansile (blown out lesions) or non expansile

“Epithelial tissue” (malignant)
Carcinoma

(slightly) expansive lesion
1A, short transitional zone with defined margin

- 1A, not purely radiolucent (has peaks and valleys/ridging inside)
- Little bit of expansion
- Speckled calcification (snowflake) : Internal matrix not fully radiolucent
** Possibly an endochondroma

- Eccentric (off centered)
- Slightly expansile, radiolucent, short tranzitional zone, well defined, and benign
- A little “scalloped”
- Cortical destruction
- Geographic, probably benign, slow growing
What is traumatic determinism?
Patient has a trauma and finds something more sinister on the film (disease in bone)
What does “Curitage” mean?
Scrape out
Some lesions may be GROSSLY expansile… what is an example?
Blow out lesion

Soap Bubble Geographic Lesion
- Giant cell tumor (ages 20-40)
- Started in metaphysis
- “Blow out lesion”
- Geographic
Giant cell tumor occurs in what ages?
20-40
An osteosclerotic lesion is NOT ….
a GEOGRAPHIC lesion
Expansile or non expansile determien
Geographic lesions
A larger zone on a geographic lesion would most likely indicate what?
A benign tumor
Geographic Lesions, name the whole list
- uni or multi compartmental (soap bubble), can sometimes cause ridges on cortex
- Centric or Eccentric
- Expansile vs Non expansile
- Well defined or poorly defined (transitional zone)
- 1A, 1B, 1C
- Thin/Thick Osteosclerotic Margin
- Large: Benign
- Internal Matrix (stuff inside; internal composition) - radiolucent, speckled calcification, isodense (fibrodysplasia) with medullary cavity
- Isodense: Internal matrix has same desnsity as medullary cavity
- Tumors: Malignant or Benign
- Tumor Like Lesions: (can be dangerous) - full of plasma fluid (as opposed to cells)
- Osteomyelitis: Bone infection - no respect for anything (joints) unlike tumors, DONT stop at subchondral bone, would continue to joints.
How can you tell the difference between Osteomyelitis and a tumor?
Osteomyelitis has no respect for joints unlike tumors, it does NOT stop at subchondral bone, it will continue to the joints

Punched Out lesions
- Well defined with NO sclerotic margin 1B
What usually occur in flat bone, especially in cranial vault, and are usually part of Myelomatosis?
Punched out Lesions

What does Monoclonalgamopathy produce?
Immunoglobulin w/ no antigenic stiumulus
** Skull is a common place for punched out lesions
Give a few characteristics of Moth Eaten
Small much more numerous holes (few mm in size)
- Ragged border/wide zone of transition (cant tell where it ends)
- RAPID GROWTH
- Larger holes than permeative
- Holes in the Haversion Canals

What 2 diseases are associated with “moth eaten” appearance?
Osteomyelitis : Common cause of mothy osteomyelysis
or Malignant: Osteosarcoma
- Metastisis doesn’t involve periosteum
If we can see the moth eaten appearance, where is it in the bone?
Cortex
What is the MOST COMMON primary bone malignancy? ***
MULTIPLE MYELOMA ****
test
What are the list of causes of Moth Eaten Osteolysis?
- Multiple Myeloma
- Mets (very common cause)
- Ewings Sarcoma
- Lymphoma
- Osteomyelitis
Does Mets start in the bone?
no
Does lymphoma start in the bone, or does it normally spread there?
Normally spreads there
Describe Ewing’s Sarcoma:
Primary bone malignancy, classified as a round cell malignancy
- 4th MOST COMMON Primary bone malignancy
- Primarily in CHILDREN

Left side
(right side is permeative)
Permeative Osteolysis characteristics:
- Ill-defined
- “worm holes”
- WIDE zone of transition
- Margins are fine vs ragged
- Almost always, MALIGNANT

What implies aggressive malginancy?
Permeative Bone
What is something special about permeative pattern in the diaphysis?
This is the worst possible sign one can see, mostly malignant in bone tumors
Permeative Lesions are normally associated with what?
- Lymphoma
- Ewing’s Sarcoma
- Myeloma
- Osteomyelitis
- NEUROBLASTOMA (Mets)
Where does neuroblastoma come from?
(mets) comes from Sympathetic Tissue (from adrenals) Happen in children under 5
- Strong tendency to metastasize to bone
- Can also be moth eaten
What is the only moth eaten look that is not malignant? ***
test
OSTEOMYELITIS
Geographic lesions in bone cannot ______ ?
Kill within months, it takes many months to years
What is a periosteal reaction?
Stimulus for new bone pathologically
- Extension of blood, pus, or tumor cells.
- Periosteum being stimulated when it shouldn’t (lift/push periosteum away from bone)

When do you see a periosteal reaction?
It has a 10-21 day latent period for Identification
- If there is a trauma or infection, this could take a couple weeks to see
What are some irritants that can give a periosteum reaction?
Hyperemia, inflammation, and edema (irritate bone)
what are the 3 patterns of new bone formation?
- Solid
- Laminated/Onion Skin
- Spiculated
* These are productive patterns that periosteum is PRODUCING BONE

Can periosteum act pathologically?
YES
What is another aggressiveness indicator?
Periosteal Reaction
- Solid = Most Benign (Codman’s)
- Laminated/Onion Skin
- Spiculated (hair on end) = MOST AGGRESSIVE

Describe a single layer periosteal reaction:
SINGLE layer periosteal new bone**
- Runs longitudinally parallel to bone
- Typically Benign
- Can be Localized or DIFFUSE
*CAN respond to insult, irritation, etc.

Describe Lamellated Periosteal Reaction:
Onion Layers (mult. Solids)
- Essentially a few “Solid” periosteal reactions on top of eachother

Describe a Spiculated Periosteal Reaction:
Going perpendicular to the bone, looks like rays of sunlight

Explain what happens during Codman’s Periosteal Reaction:
Happens at peripheral margin of pathology (not really a separate type, but happens with the other types)

Describe what Osteoid Osteoma is and what can it cause?
Very LOCALIZED solid periosteal reaction
**** Benign bone NEOPLASM
- Very dense and looks like area of cortical thickening
- Very COMMON; classic bone forming bone tumor

Can Infection cause a periosteal raection?
YES
Describe Eosinophilic Granuloma and what it can do:
- Granulation tissue is stimulated by chronic inflammation, only; Associated with eosinophilium
* Cause of COMPRESSION fractures in the spine
- (CAN CAUSE PERIOSTEAL REACTIONS)

What is Granulomous?
Chronic inflammatory
- Produce Granulation tissue
- Response of host being chronically inflamed
Describe Hypertrophic Osteoarthropathy and what it can do:
It is “ALL OVER”
- TOO MUCH growth of bones and joints
- Primary and Secondary
SECONDARY: COMMON*, diffuse, secondary–> lung cancer
*** CAN CAUSE PERIOSTEAL REACTION

Describes Varicosities in the lower extremities:
Accumulate in the bone leading to BONE PAIN in varicose veins (predominantly: _Tibia, Fibula, and Metatarsals**)_
- Blood pools under periosteum due to poor venous drainage
- Bone expresses venous disorder
***** CAN CAUSE PERIOSTEAL REACTIONS****

Describe Fracture Healing:
Callous Formation helps produce a new collar of new bone
- Periosteum contributes to fracture, builds shell around fracture site
- Can be runner with fatigue stress fracture or trauma
_**** CAN CAUSE PERIOSTEAL REACTION *****_

What are the 2 types of Solid Periosteal Reactions?
- LOCALIZED: Direct Stimulus from an underlying bone lesion (intrinsic); mc fracture healing, infection and benign bone neoplasm
- WIDE SPREAD: Systemic diseases and the periosteum is reacting; mc Hypertrophic osteoarthropathy


Pic on the RIGHT: Looks like area of cortical thickening; solid periosteal reaction is less dense MOST OF THE TIME (not in this picture).
It is hard to see tumor in growht, but patient would have “Point Pain” at growth site
NO TRAUMA HISTORY
Describe some key features of primary hypertrophic osteoarthropathy/pachydermoperiostitis:
Skin thickening and PERIOSTEUM
- 3-5% are primary; rest are secondary
- Digital CLUBBING (soft tissue thickening on tips of fingers)
- Progressive for 10 years and then regresses
- *** Radiographically diffuse widespread symmetrical periostitis involving diaphyses and metaphyses

Describe the key points of Secondary Hypertrophic Osteoarthropathy:
Diffuse, solid periostitis in an adult perineoplastic syndrome
** Mesothelioma, Hodgkin’s, Cystic Fibrosis, Pulmonary Metastasis, Cyanotic Heart Disease, Chron’s
- A TUMOR producing hormones (cushings disease)
- Up to 12% of patients with bronchosarcoma (lung cancer) maybe first symptom
- Patient with Lung Cancer (no symptoms)

Describe the key points of Thyroid Acropachy:
Usually seen after treatment for hyperthyroidism when patients are euthyroid or hypothyroid
Findings: Exopthalmos digital clubbing, pretibial myxedema and periostitis similar to secondary HOA

Describe Venous Stasis:
Lower extremity almost exclusively, associated with varicosities which
May Contain: phleboliths, periostitis involving distal tibia, fibula, and possibly metatarsals

Infantile Cortical Hyperostosis (Caffey’s Disease):
Uncommon disorder of infancy middle of 1st year
- Abrupt onset with fever hyperirritability and soft tissue swelling especially over mandible
- Children with BONE PAIN
- MANDIBLE, CLAVICLE, RIBS, PERIOSTITIS (can be extreme enlarged bone.

Describe Hypervitaminosis A:
Can occur in both children and adults, vomitting, headache, drowsiness and irritability
- Periostitis, involving tubular bone: ulna and metatarsals, clavicle, tibia, and fibula

Describe Scurvy
Periostitis may occur in children related to subperiosteal bleeding related to capillary fragility associated with Hypovitaminosis C

Describe Battered Children
Multiple areas of solid periosteal new bone associated with multiple fractures at different stages of healing

Describe Acromegaly
Excessive growth hormone production can stimulate solid periosteal new bone formation

Describe Leukemia:
Multiple areas of bone destruction associated with adjacent periostitis

What is a laminated Periosteal Reaction?
AKA: Lamellated, layered, onion skin
- Alternating layers of parallel/solid bone separated by thin radiolucent layer (multiple layers)
- WIll NEVER form full cortex
What is the most common disease associated with a “Laminated Periosteal Reaction?”
***test***
EWINGS SARCOMA****
Most Common: Eosinophilic granuloma, Osteomyelitis, Leukemia - Most common under 30
- *FIRST DECADE OF LIFE******
- Usually localized, intrinsic
- Most likely will be found in _DIAPHYSIS**_

What is the TOP 5 Primary Malignant bone cancer?
M.O.C.E.F.
- Multiple Myeloma
- Osteosarcoma
- Condrosarcoma
- Ewings
- Fibrosarcoma
**** ALL ORIGINATE IN BONE = PRIMARY *******

What is the most aggressive periosteal reaction?
Spiculated
AKA: Perpendicular, brushed whiskers, hair on end, and sunburst
- Sunburst is characteristic of osteosarcoma
How does the spiculated periosteal reaction occur?
Growth is so quick that periosteum being lifted so fast (5-6 weeks) doesn’t have time to fill in, so it leaves traces (hairs)
** Rapidly Growing Lesions
What are the main characteristics of Spiculated Periosteal Reaction?
Fine, linear spicules oriented perpendicular to cortex
- All outgrowth happening under the periosteum

Spiculated happens faster than solid periosteal layer?
t/f
TRUE
What is the most common disease to have spiculated Reaction?
Osteosarcoma,
can be leukemia, but it can also be Solid, Lammelated, or Spiculated
Ewing’s is from what type of cells?
ROUND
Osteomyolitis can induce what type of periosteal reaction?
ANY of them
What are the big malignant neoplasms?
- Ewings
- Osteosarcoma
- Chondrosarcoma
- Fibrosarcoma
- Non-Hodgkin’s Lymphoma
- Leukemia
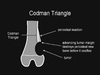
Where does Codman’s Triangle/Cuff occur? What are the key features of it?
Occurs at PERIPHERY of fast growing lesions
- Typically with an AGGRESSIVE REACTION
- Can be SOLID or LAYERED/LAMELLATED
- USUALLY at edge of SPICULATED LESION
**** Commonly MALIGNANT, but can be with any type ***

Left: Spiculated and moth eaten
Right: Spiculated
What is the summary features of PERIOSTEAL REACTIONS? *** know this next picture and you’ll be good

Less trabecular bone =
Thinning (osteoperosis is a classic example)
Accentuated Trabecular Bone =
Can happen because of production of more trabeculation or by compressing into smaller spaces
Describe what happens during Padget’s disease…
Osteoclasts are thinned out by osteoclasts, but when they rebuild, it is too thick
This creates a thick cortex, and weaker bone (poor quality osteoids)
- Hemolytic Anemia then follows

With loss of trabeculation or osteoperosis, what happens to bone?
THINNER CORTEX, greater potential for fracture
30-50% less seen on film
**** OSTEOPENIA: soft bone, looks like soft tissue on film

Coarsend/Prominent Trabeculation:
Over production of trabecular bone, or by squeezing and compression
* Can happen locally or widespread depending on unerlying pathology
*Can do this by compressing or squeezing bone, locally, widespread, or diffuse
What are some diseases that have a coarsened/prominent trabeculation look?
Hemolytic Anemias (sickle cell), Paget’s disease (overproducing trabecular bone will be very thick looking)
** HEMANGIOMA ***
Most common benign bone tumor
What’s the most common benign bone tumor?
HEMANGIOMA

In the case of a coarsened/prominent trabeculation, if there is hemolytic anemia, what will occur?
Increase in red marrow volume (in diaphysis of tubular bones)
RBC production increases in medullary (small cavity), this will compress trebeculation, creating bigger gaps between them, thus….more TRABECULATION grows in gaps

What is the single sentence summary of Paget’s Disease?
Overproduce trabeculae and makes them thicker (2 mm)

What is Hemangioma? (one sentence)
Benign vascular tumor –> Compresses trabecular bone


_Corduroy Cloth Appearance**_
- Regional Squeezing
- Trabeculae are thicker going verticle
- Vessels are grossly EXPANDED, compresses trabeculae
- Sometimes it will be in PEDICLES and not verticle
- LOCALIZED
_** HEMANGIOMA_
In flat bone, what would the appearance of hemangioma be called/look like?
Hub and Spoke

Paget’s Disease (Osteitis Deformans)
- REGIONAL overproduction
- Makes bone SOFTER**** despite THICKER looking trabecular (check out left acetabulum)
- NO pain with PAGET’S
- Femur tends to bow LATERALLY (Saber shin deformity)
How common is Paget’s?
Single digit (common)
How does the trabeculation increase in paget’s?
Via overproduction, NOT be squeezing
Can Paget’s lead to DJD?
YES

COARSE TRABECULATION
(NOT*** spiculation **)
- Thalassemia Skull: Course trabeculation by compression, again, NOT spiculation (dont confuse the 2)
- “Hair on End Appearance”
- Stops at EOP because of the red marrow above (no hematopoietic potential), and the yellow marrow below EOP
- Expands medullary cavities, facial bones, and destroys sinuses
What is Coarse Trabeculation derived from?
Hemolytic Anemia
Describe the cortex of Coarse Trabeculation…
Actual Cortex is very thin, and is at edge of “hair”; skull EXPANDS!
- Increase in pressure pushes out cortex
- _DERIVED FROM HEMOLYTIC ANEMIA****_

How can bone bend?
Softening disease,
- Paget’s,
- Polyostic fibrous dysplasia,
- Osteomalacia
**** test ****

BRACHYDACTYLY
- Short fingers, short toes
- Patients with sickle cell are prone to microvascular occlusion; cut off blood flow to bone = Avascular Necrosis –> Leads to stunded bone growth

Shape change = POLYDACTYLY
**** Ellis van Crevald Syndrome: Patient will have an extra digit off the hand and or foot, usually symmetrical and will have a seperatie bone off the base of 5th metacarpal/metatarsal

SHEPHERD’S CROOK DEFORMITY
- Bone softening disease (osteomalacia, rickets)
- _Femoral neck angle > 90****_

ERLENMYER FLASK DEFORMITY
- Typically seen in big tubular bones
- Many Pathologies
- EXPANISON of proximal and distal diaphysis
- *** ONLY IN BIG TUBULAR BONES (short ones become rectangles)

MADELUNG’S DEFORMITY
- Have a hard time picking up things (ROM changed)
- Impacts ossification center at distal radiusarticular surfaces
** Caused by: Many things, but commonly Salter Hairris Fracture Type 5 in a peds patient, if it happens via TRAUMA
When madelung’s deformity is idiopathic, what happens?
It happens in teenage girls
Madelung’s can be …..
genetic or acquired
What will Madelung’s create? How does it happen?
with FOOSH injury that damages growth plate in peds patient
- Sometimes idiopathic in teenage girls, dwarfism, Turner’s children
- Will affect grip strength and creates a V shape
- PAINFUL

Bones can either be what?
Increase in density (Osteoblastic, OSTEOSCLEROSIS)
Decrease in density (Osteoclastic, OSTEOPENIA)
Localized/Regional or Widespread/diffuse/Global
- Global Osteopenia
- Osteopenia around joint
*** Bone density changes are extremly common**
Describe Osteosclerosis/Hyperostosis:
Increase of amount of bone matrix in given volume of bone
X RAY APPEARANCE: Bone density increased
-
Cortex Thickens = Periosteal growing
- This causes patient to become anemic because there isn’t enough marrow to produce RBC
- Bone Marrow Cavity Narrowing = Endostosis growing and trabecular thickening
What is the Etiology of Osteosclerosis/Hyperostosis?
- Inflammation or Granuloma (chronic)
- Trauma & Fracture Healing
- Tumor or Tumor Like Lesion

Osteoperosis (Osteosclerotic)
- Cannot transition from primary –> Secondary Spongiosa
- Diffuse Osteosclerosis (Dramatic increase in density)
- Not really common

OSTEOPOIKILOSIS
- Regional (periarticular) Osteosclerosis
- No increase in bone density in ilium
- Generally an accidental finding-patient has no complaint
- _HAS PATTERN, and AROUND JOINTS**_
- Not really around extremities, just joints
AKA: “Patchy Osteosclerosis” “Bone Islands”
* NO SIGNS OR SYMPTOMS *

IVORY VERTEBRA
- Multifocal Osteoblastic metastasis (Not around Joint)
- Probably PROSTATE/BREAST cancer spread to bone via bloodstream –> Bone marrow
- Stimulate OSTEOBLASTS
- Very random; NO uniform distribution on both sides
- FOCAL AND RANDOM
Define Osteoperosis:
The bone matrix or osteoid specific deficiency
Both of the organic material & calcium are decreased, but the ratio them is still normal
What is the X ray appearance of Osteoperosis (Osteopenia)?
Bone Density is decreased local/general
- The cortex becomes thinner, the trabeculae become thin and decreased number. Bone begins to look as gray as soft tissue
- PATHOLOGICAL fracture
What is the etiology of Osteoperosis/osteopenia?
- Common in elderly and immobilization
Pathology: Hormonal (PTH, etc) / Vitamin deficiency
What do we look at with Osteoperosis/Osteopenia?
- Soft tissue first
- Should look GRAY
- If there is thin cortex: They will have loss in strength

REGIONAL/LOCALIZED OSTEOPENIA
- Very PAINFUL (usually follow trauma) - FOOSH
- Crps/smps/rsds/Sudeck’s atrophy
- Rhuematoid can cause this
- Para-articular Osteopenia (sympathetic nerve pain)
* Bone density on right significantly decreased
* Rheumatoid Arthritis can also do this, but it would be bilateral (80% of the time)

DIFFUSE OSTEOPENIA
- childhood osteomalacia/rickets ( lose zone of provisional mineralization) mostly from renal disease
- Soft tissue looks gray: (GOOD)
- Bone tissue looks gray: (BAD); should look white
-Cortex too thin

Combination of osteosclerosis intermixed with areas of radiolucency
- Have both osteoclastic and osteoblastic activity going on at the same time
- Osteoclasts tend to win out leading to decrease in bone density
Avascular necrosis is most common where?
Femoral Head
When chondrocytes die, this causes what to happen?
Cartilage Degeneration (DJD)

* Small and large patchy bone destruction area as well as increased density area in pelvis, lumbosacral vertebrae and bilateral femur.

Very COMMON
** AVASCULAR NECROSIS ***
-
Density change coming from repair
- Use osteoclast to remove dead bone (radiolucency)
- Use Osteoblasts to build new bone (radiodense/radiopaque)
- Osteoclastic Activity usually higher than osteoblastic activity
So if patient walks, femoral head will suffer (femoral head changing shape) = DJD
What is common cause of mixed density change in the femoral head?
Avascular Necrosis

** MIXED DENSITY change on CT scan
What can plain film reveal about soft tissue?
Abnormalities
Soft tissue masses may be _________ ?
Tumor associated, soft tissue swelling around the joints, traumatic hematoma, infectious abscess, calcification, or ossification of soft tissue
What is the “GOLD STANDARD” for soft tissue?
MRI
Fat is not as _____ as muscle is?
DENSE

Soft tissue enlargement of the knee
- Peripheral Chondrosarcoma - Originated from benign OSTEOSARCOMA
What is related to peripheral chondrosarcoma?
Soft tissue enlargement and speckled calcification (malignancy)

Soft tissue swelling/enlargement - Heel pad calcanealapophysis fracture
- Not abnormal for calcaneous to be osteosclerotic
_*** SALTER HARRIS 3 FRACTURE ****_ (pictured)

Calcinosis Cutis
- Progressive Systemic Sclerosis (Scleroderma) –> soft tissue calcification
*** When patient has Rheumatoid type autoimmune condition - lupus, scleroderma, dermatomyositis, polymyositis
Define Calcinosis Cutis…..
Calcification around joints
Sclerosis in soft tissue =
Scarring

Calcinosis Universalis - Dermatomyositis
* AUTOIMMUNE DISEASE
* MUSCLE FASCIA INFLAMMATION
- Weakness and fatigue, muscle fascia CALCIFIES
WHat is calcinosis?
Soft tissue calcification relatable to autoimmune disease
Describe the soft tissue calcification (Metastatic)?
Elevated serum Calcium (Hypercalcemia)
- HPT : Hyperparathyroidism
- Hypervitaminosis D 40,000 - 50,000 IU for months
- Milk Alkali Syndrome > 1 gallon a day
Describe soft tissue calcification (Calcinosis)?
Cutis (just in skin)
- Circumscripta (local, but deeper than skiin around joints), universalis (very wide spread; Extensive calcification)
- Normal serum calcium but they have an AUTOIMMUNE disease (rheumatoid)
What is the most common Soft tissue calcifciation?
_Dystrophic**_
- <em><strong>Scar Tissue</strong></em>
- NORMAL serum calcium, but DONT have autoimmune disease
- Happens a lot in chest
Post tramautic myositis ossificans
Impact sports, car accident, falling
- Happens in large muscle groups
- LARGE BLOOD CLOT IN SOFT TISSUE ****
- Can scar, dystrophically calcify bone
* May even develop corticol bone

Hetertopic Ossificans
- Quadriplegia****
- P*atients with total hip arthroplasties can get this (due to trauma and manipulation of soft tissue)
** Soft tissue ossifies, but no macrotraumatic event

Fibrodysplasia Ossificans Progressive “Munchmeyer’s Disease”
- Most don’t live beyond mid-30’s
- Ossification of SKELETAL MUSCLE ONLY
- Turns skeletal muscle into bone (muscle ossifying)
- Inability to breathe
Most benign tumors happen when?
Before age 30
Radionuclide bone scan =
WHOLE BODY
is MRI full body?
no, its REGIONAL
CT will find ______ of spinal trauma?
100%
Nucelar Medicine has great ____ but lousy _____
Great sensitivity
Lousy Specificity
What does Diagnostic Nuclear Medicine measure?
What the patient is emitting = Endoradiology
What is a synonymous term for nm scan?
Scintigraphy
What is Methyline Dipohsphate used as?
As a carrier for radioactive substance (Tc-99m) into bloodstream
Technetium 99m MDP (methylenediposphonate) most widely used for —
bone


