Written Exam 2 Flashcards
What does the skin do?
- Protective (barrier)
- Minimize water loss
- Prevent entry of pathogens
- UV radiation
- Physical forces
- Sensory
- Body temp regulation
- Produce vitamin D
What layer of the skin are epithelial cells found?
Epidermis
(epi = epi)
Name and describe the layers that make up the skin
- Epidermis (Epi = on top of)
- Dermis
- CT under the epidermis
- Hypodermis (hypo = below)
- CT under the dermis
- Lots of adipose tissue!
- CT under the dermis

Explain the difference between thick skin and thin skin and where each are found
-
Thick skin:
- Found in palm of hands and bottom of feet
- Lots of keratinized epithelium
- thick epidermis
- Varies a lot (differentiation point between thickness of skin)
- smaller dermis
- Found in palm of hands and bottom of feet
-
Thin skin:
- Found everywhere on skin but palms of hands and bottom of feet
- Skinnier epidermis
- Not as much keratinized epithelium
- Thicker dermis

What is skin cancer and why can there be several types?
Cancer = uncontrolled cell growth
How can there be several types?
There is more than one type of cell in the skin
What are the cells found in the epidermis, what type of cancer can be found in each cell type and where they are located?
- Basal Cells = Basal cell carcinoma
- Keratinocytes = squamous cell carconoma (flat c)
- Squamous cells = squamous cell carconoma
-
Melanocytes = melanoma (pigmented moles)
- In basal layer
-
Merkel cells = Merkel cell carcinoma
- In basal layer
-
Langerhans cells = Immune cells in epidermis
- Dendritic cells (stratum spinosum)

What is the function of the tactile cells?
Tactile (Merkel) cells
- located in basal layer throughout. Sensory nerve endings attach to these cells

What is the following layer of the epidermis called and what are the distinct characteristics?

Stratum Basale
(layer base)
- One cell layer thick
- cuboidal or columnar cells
- contain demidesmosomes to attach to CT under
- mitotic cells - stem cells, production of new cells
- contain desmosomes to attach to each other

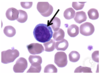
What is the following layer of the epidermis called and what are the distinct characteristics?
(black arrow)

Stratum spinosum
- No hemidesmosomes (does not attach to CT)
- Has desmosomes (attach to each other)
- Some mitotic cells
- Thicker in thick skin than thin
- Active cells => makes protein (keratin)

Explain the function/process of keratinocytes and where they are located in the epidermis
Keratinocytes in the stratum spinosum
>>>>>
producing keratin
>>>>>
Makes up the intermediate filaments (made of keratin) in the epithelial cells of the skin
(tonofibrils) = special name
Remember: intermediate filaments are involved in intracellular adhesion
Which type of junction involves the intermediate filament?
Desmosomes
= integrins

Explain the components in the following EM slide

Keratinocytes in the stratum spinosum
- Tonofibrils of keratin = dark lines
- intermediate filaments
- Cytoplsamic extensions
- Desmosomes
- electron dense

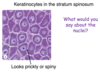
Describe the following slide

Keratinocytes in the stratum spinosum
(looks like a spine = prickly)
- What would you say about the nuclei?
-
Euchromatic = active
- DNA dispersed
-
Euchromatic = active
- Looks prickly or spiny = cytoplasmic extension
What is the following layer of the epidermis called and what are the distinct characteristics?
(black arrow)

Stratum granulosum
- squamous shape
- Only 3 to 5 layers thick
- Cells develop a lipid envelope (water resistance)
- Cytoplasm has Basophilic masses
- Hemotoxylin staining

Explain a summary of the differentiation of cells in the stratum granulosum

-
Cells contain many keratohyaline granules
- Contain several proteins, including profilaggrin
- Granules stain w/hematoxylin = dark color
-
Cells also contin many lamellar grandules
- contain several substances, including lipids
- The nucleus and other organelles degrade and the cells begin to die in this layer

Explain a summary of the keratinization of cells in the stratum granulosum
-
Proflaggrin is proteolysed into multiple filagrin monmers.
- Free filaggrin binds to keratin intermediate filaments, causing aggregation into macrofibrils
- intermediate filaments aligned in tightly packed parallel arrays
- Free filaggrin binds to keratin intermediate filaments, causing aggregation into macrofibrils
-
Lipids and other substances are secreted from lamellar granules
- forming a lipid barrier encircling the cell
- Lipid + filaggrin + keratin matrix = important skin barrier

Explain the end result of keratinization in the stratum granulosum layer of the epithelium
End result of keratinization -> cornified cell
Compressed keratin + filaggrin
-
Contains lipid envelope:
- Prevents abrasion
- Prevents desication
- Protects form infection

What is the following layer of the epidermis called and what are the distinct characteristics?
(black arrow)

Stratum lucidum
- light layer above the stratum granulosum
- ONLY in thick skin
- Cells that lost their organelles
- Contain desmosomes = cells still attached to each other

What are the following structures in this slide?

stratum lucidium = light layer
stratum granulosum = dark layer

What is the following layer of the epidermis called and what are the distinct characteristics?
(black arrow)

Stratum corneum
- Very thick in thick skin and very thin in thin skin
Non nucleated, keratinized cells called squames or cornified cells
- Contains loose desmosomes
- Cells at surface begin to sluff off as the desmosomes break down
- Keratin dust

Where are melanocytes located?
What is the function of melanocytes?
- Melanocytes = dispersed throughout the stratum basale
- Melanin is packaged in small special vesicles called = melanosomes
- Melanocytes have cytoplasmic extensions or dendrites. The melanosomes mature and move to the tip of the dentrite
- The tip of the dendrites with the melanosomes is engulfed by keratinocytes and the melanosomes move towards the nucleus
- Produce melanin and transfer it to keratinocytes
- Tip of the melanocyte gets moved/bit off and goes to the keratinocyte

What is the following cell?

Melanocyte
Can tell it is a melanocyte because of the hollow (clear area)
- Error from the tissue processing
Melanin capping the nucleus of a keratinocyte

Why does melanin accumulate in this supranuclear cap?

Protects DNA from UV radiation
- All skin color has the SAME DENSITY of melanocytes, however there may be LESS MELANIN IN KERATINOCYTES
What are these brown stained cells?
Langerhans Cells
- Immune cells
Type of dendritic cells
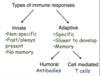
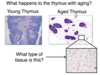
Explain how langerhan cells, or dendritic cells, are involved in immune response
Immune cells
Phagocytize antigen
>>>>>
move to the lymph node
>>>>>>
Present the antigen to lymphocytes
START THE IMMUNE RESPONSE
DEFECTS IN CUTANEOUS BARRIER FUNCTION CAN PREDISPOSE AN INDIVIDUAL TO SKIN DISEASES, SUCH AS ATOPIC DERMATITIS. A GENETIC DEFECT CAUSING THE LOSS OF WHICH OF THE FOLLOWING WOULD MOST LIKELY CONTRIBUTE TO THIS?
Filaggrin
rash development and holes in skin
Because it deals with keratinization and is the cutaneous barrier

What features can be found in the dermis of the skin?
Blood vessels
Connective tissue
Hair
Nerves
Sebaceous and sweat glands
Sensory receptors
What do you notice about the interface between the epidermis and dermis?
What are their functions?

Dermal Papilla = bumps up from the dermis
Epidermal Ridge = Pokes down from the epidermis
Strength - ie reinforce the dermal-epidermal junction
What are the two following layers in the thin skin sample
-
Papillary Layer = dermal papilla - up from dermis
- Fine collagen, elastic fibers with
- MORE CELLS
- Loose CT
- Fine collagen, elastic fibers with
-
Reticular layer = network of CT
- Course collagen, elastic fibers
- LESS CELLS
- Dense Irregular CT
- Course collagen, elastic fibers

What type of collagen is found in the dermis?
Type I = lots in the reticular layer
Type III = Reticular fibers. Lots in the papillary layer (dermis)
Type IV = In the basal lamina/basement membrane (papillary layer = dermis)
Type VII = Anchoring collagen (papillary layer)
Note: Basement membrane is considered part of the dermis
basal lamina = basement membrane = dermis
What are the two types of sensory receptors in the skin?
Nerve Endings
- Not encapsulated
-
Encapsulated (mylinated)
-
Collagen and modified schwann cells
- Schwann cells = form myelin sheath
-
Collagen and modified schwann cells
What is the function of free nerve endings and where are they located?
Free nerve endings = sensory neurons
Location = epidermis
Function: Sense pain, temperature, itching, light pressure (touch)

What is the function of Merkel cells and where are they located?
Location: Scattered throughout basal layer of epidermis which is connected to the
merkel (tactile) disc
Function: Sense light touch
Non-encapsulated = simple nerve ending

What is the function of root hair plexus nerves? Where are they located?
Location: Nerves wrapped around the plexus of a hair
Function: sense hair movement

What are the two types of corpuscles that are found in the dermis and where in the dermis are they located?
-
Meissner corpuscle
- Sits in the dermal papilla
-
Pacinian Corpuscle
- Deeper in the dermis

What is the following feature?

Meissner Corpuscle
- Extremely difficult to see and will be super lucky to find one
- Sits in the dermal papilla
- Unmylinated nerve ending
- Surrounded by modified schwann cells and capsule
- Function: feel shapes, detail
- Location: Hands, fingers, lips, tongue and sole of the feet

What is the following feature and explain function, location, details

Pacinian corpuscle
Very easy to see in a section of your skin
- Location: Deeper in the dermis
- Axon w/modified schwann cells
- Function: Course touch, pressure and vibrations
- Not too many but due to large capusle they can sense when capsule is moved

A 34 year ld female is stung by a bee. She develops urticaria (hives) and pruritus (itchiness). What is going on in the dermis of the skin to cause this reaction?
Mast cells degranulate and release histamine
mast cells are in the skin!!
What causes itching?
Free nerve endings
- Histamine release
- Histamine binds to H1 receptor
- Itching feeling
Explain the anatomy around the hair follicle
-
Arrector pili muscle = smooth muscle
- Body temp. regulation
- Sympathetic nervous system (involuntary)
- Outside in:
- Invagination of the epidermis
-
External rooth sheath
- Sheaths the root of the hair, not involved in the production of the hair
-
Matrix
- Under the sheath
-
Hair pulp, Dermal papilla
- nutrient/blood supply to matrix
- CT with blood vellels

Explain the anatomy of an oblique section of a hair follicle

Oblique section of a hair follicle
- Cells move up and are keratinized to form the hair root and shaft
-
Matrix
- Dividing epithelial cells and melanocytes
- Because hair has color to it
- Epithelial tissue = avascular, cells need nutrients from the dermal papilla
- Dividing epithelial cells and melanocytes
-
Dermal papilla
- CT with blood vessels
- Supplies blood to the hair (to matrix)
- CT with blood vessels

Explain the anatomy of a cross section of a hair follicle

**Do not see matrix here
- Connective tissue sheath
-
Glassy membrane
- Like the basement membrane
-
External root sheath
- Invaginated epidermal cells
-
Internal root sheath
- Comes from the matrix with a softer keratin
- Not from head or skin
- Comes from the matrix with a softer keratin
- Hair (keratinized cells)

What is the following feature and where are they located?
Why does the feature not stain?

Sebaceous gland
- These are epithelial cells that make up the gland
- Produce: sebum
- Lined with undifferentiated epithelial cell differentiate into sebocytes
- Then lined with Basal lamina
- Outside layer: Connective tissue capusle surrounds the gland
- Location: Face, forehead, scalp
Does not stain: Cytoplasm filled with fat droplets
Sebum = waxy mix of cholesterol and fat that coat the skin and hair

How is sebum secrted into the hair follicle with sebaceous gland?
Holocrine secretion

What type of glands are sebaceous glands?
Branched acini

Name and the following features in the image and where they are located

- Duct opens to surface
- Eccrine sweat gland (All over the body)
- Duct opens to hair follicle
- Apocrine sweat gland (axillary and perineal regions)

What is the following structure?
What are the following features in the structure

Eccrine sweat gland
- Small lumen
- Cuboidal epithelium with underlying myoepithelial cells
- Duct

What is the following structure?
What features make up the structure?

Apocrine sweat gland
- Large lumen
- Cuboidal epithelium with underlying myoepithelial cells

what type of tissue is cartilage?
Connective tissue
What are the types of cartilage and where are they found?

-
Hyaline (blue)
- Articular cartilage (ie. Joints)
-
Fibrocartilage (red)
- Vertebral disks
-
Elastic (purple)
- Ear

What is the following features in the image?

-
Perichondrium
- Peri = around
- chondro = cartilage
-
Hyaline cartilage
- Dark spots inside cartilage = chondrocytes
- cells of cartilage
- Dark spots inside cartilage = chondrocytes

What is the following picture of? name and describe the features of the tissue

Hyaline cartilage
- Very glassy
- Lots of extracellular matrix
- Contains lots of condracytes
Does the extracellular matrix in the perichondrium look the same as the ECM in hyaline cartilage?
Describe the tissues in the cartilage layers

NO
- Perichondrium:
- Dense CT
- Type I collagen
- Hyaline cartilage:
- Type II collagen fibrils
- Lots of ground substance
- forms a gel

Why does the extracellular matrix in hyaline cartilage appear more purple?

Blue + pink = purple
-
Aggrecan = proteoglycans
- Protein + GAG (lots of negatively charged sulfates)
- Proteoglycans!!! Lots of branching (purple in color)
- Protein + GAG (lots of negatively charged sulfates)
-
Hyaluronic acid
- Glycosomino glycan in the ground substance (GAG)
- Blue color
-
Type II collagen
- Fibers = more pink

Why is the extracellular matrix in hyaline cartilage like a gell?

Lots of negatively charged sulfates and lots of water
-
Aggrecan
-
Protein + GAG
- Lots of negatively charged sulfates
- attach/attracted to water molecules
- Lots of negatively charged sulfates
-
Protein + GAG
Becomes a high water content gel

What is the function of the type II collagen and the ground substance in hyaline cartilage?
-
Collagen = gives it tensile strength
- Do not want to rip a part
- Type I = strength
- Type II = lots of strength in cartilage (prevents ripping)
-
Ground substance = makes it resistant to pressure
- want some squishiness
What type of cells are in each of the layers of hyaline cartilage?

-
Perichondrium =
- Fibroblast or fibroblast like cells in the perochondrium
-
Hyaline cartilage =
- chondrocytes in the lacuna (empty space like a lake artifact)

Why does it take a long time to repair damaged cartilage?
- Cartilage is avascular (long time for repair)
- Blood supply is in the perichondrium
-
Chondrocytes have low metabolic activity and limited ability to divide
- pretty static
- Chondrocytes still need nutrients, get it in the perichondrium
Where do new chondrocytes and matrix come from?

fibroblast like cells
>>>>>>
differentiate into chondroblasts
(adding more cartilage on top of other cartilage)
(apositional growth)
Can divide and lay down matrix
(some ability for chondrocytes to divide)
>>>>> Intersititial growth (inside cell)

What is the difference between hyaline, elastic and fibrocartilage?
-
Hyaline
- Type II collagen
- Perichondrium present
-
Elastic
- Type II collagen and elastic fibers
- Perichondrium present
- Ex. epiglotis
-
Fibrocartilage
- Type I and II collagen -> CT very strong
- No perichondrium present
- Ex. intervertebral discs -> super strength

What type of tissue is bone?
Connective
What are the components of bone and function? Cells and extracellular matrix
-
Cells
- Osteoblasts - remodeling
- Osteoclasts - remodeling
- Osteocytes - helps ‘maintain’ matrix
- Bone lining cells
- Osteoprogenitor cells - gives rise to osteoblasts
-
Extracellular matrix = bone matrix
- Fibers
-
Ground substance
- GAGs, proteoglycans, multiadhesive glycoproteins
What type of collagen is in bone?
Type I collagen
Lots of STRENGTH
(tendons, ligaments, bone, skin, sclera, etc)
Explain the fiber arrangement in bone tissue and its major function
- Function: STRENGTH in MULTIPLE directions
- in layers
- The fibers in bone are aligned in parallel, but oriented in different directions
- Called LAMELLAR BONE
- CONCENTRIC LAMELLAE = layers
- Called LAMELLAR BONE

What else gives bone its great strength?
Bone matrix is CALCIFIED
Type I collagen + ground substance = calcification
>>>>>>
Mineralized with hydroxyapatite crystals
Insoluble salt of calcium and phosphorus
= forms a crystal
Explain the structures of ground bone

Ground bone
because bone is so hard you cannot section it without getting ride of the calcium or grinding it down to see the sections
-
Layers of bone matrix
- each of these layers = lamella
- Osteocytes in lacunae (lake)
-
Central canal
- Contains blood supply for osteocytes in the lacunna
- ** Contains no capillaries**
-
Canaliculi
- Little channels between the lacuna in the matrix of the bone
-
osteon
- one circular bone structure

What is the following structure?

Osteocyte in a lacuna
- Dendritic process surrounded by bone matrix
>>>>>
Within the canaliculi

What happens in the canaliculi?
- Osteocytes are encased in mineral matrix that prevents diffusion of substances
- Osteocytes sit in a lacuna
Nutrients: travel from central canal to osteocytes via dendritic process
Wastes: travel from osteocytes to central canal via dentritic process

What type of intracellular communication structure aids with the transfer of nutrients from one osteocyte to another?
Gap junction
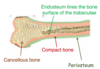
What are the types of bone?
Name and describe
-
Lamellar bone
-
Compact bone
- cortical bone = because it generally located on outer edge or cortex of bone
-
Cancellous bone (spongy, trabecular bone)
- Looks spongy and contains trabeculae
-
Compact bone
-
Woven bone
- Occurs during fetal development and bone repair. Then remodels to lamellar bone
- FASTER AND EASIER TO LAY DOWN

Explain the structure of compact bone
Contain osteon
- Contain:
- External circumferential lamellae
- internal circumferential lamallae
- interstitial lamallae
- Osteon
- Centraol canal with blood vessels and nerve

Explain the structure of spongy bone (cancellous or trabecular)
No osteon
- Lamellae = large circles
- Osteocytes in lacuna
-
Canaliculi open to surface
-
Avascular and use canaliculi that open to the surface
- get nutrients from bone marrow
-
Avascular and use canaliculi that open to the surface

What lines the surface of bone tissue?
-
Endosteum
- Lines surface of trabeculae
-
Periosteum
- lines outside of compact bone
Explain the structure of trabeculae and location of osteoprogenitor cells
-
Endosteum
-
Osteoprogenitor cells or bone lining cells
- Quiesent cells not doing much
- CT layer
-
Osteoprogenitor cells or bone lining cells
-
Periosteum
-
Osteoprogenitor or bone lining cells
- Quiesent cells not doing much
- Dense fibrous CT
-
Osteoprogenitor or bone lining cells
** Dense fibrous CT connected to epithelium via Sharpey’s fibers
- Perforating
- Connects periosteum to the bone

Explain the following structures

Stained section of demineralized bone
- Demineralized by removing the hydroxyapatite crystals
- Calcium phosphate crystals removed to allow for staining

Identify the following structures

Osteocytes
Sharpey’s fibers

Explain the process of bone remodeling
- Resting bone
- Osteocytes or hormones recruite pre-osteoclasts to bone from bone marrow
- Osteoclasts attach to bone and resorbs the bone
- Osteoclasts create a resorption lacuna and release acids and enzymes to remove the bone
- Osteoclast moves/apoptosis
-
Bone lining or osteoprogener cells turn into osteoblasts
- more cube shaped = active
-
Osteoblasts secrete bone matrix
- Lay down osteoid
- Unmineralized bone (Type I collagen that becomes mineralized)
- Lay down osteoid
- Bone mineralizes and traps osteoblasts in matrix to form osteocytes
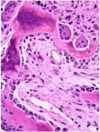
Identify the following cell types in the tissue sample


Identify the following structures in the image


Identify the following structures in the slide image


Explain the path of osteoclasts movement/remodeling through bone

Identify structures in the following slide/image

What role does osteoblasts and osteoclasts, or bone remodeling, play in the development of osteoporosis?
What exactly is osteoporosis?
Decreased bone mass per unit
volume of anatomical bone
-> Thinning bone over time
Explain the onset of osteoporosis and how bone density changes over time
**Why it is important to build up bone when you are younger so you have more bone you have to break down before getting to a critical level**

Explain a drug commonly used to fight osteoporosis, reaction and its side effects
Bisphosphonate drug inhibits osteoclasts
- Side Effect:
- Osteonecrosis of the jaw = when trauma to the bone (eg. dental surgery) occurs along with continual stress from chewing
- Bisphosphonates disrupt bone remodeling
- Bone has limited capacity for healing
What are the two types of osteogenesis
- Intramembranous ossification
- Endochondral ossification
What are the different shapes of bones?
Long bone (eg. femur)
Short bone (eg. wrist)
Flat bone (eg. skull)
Irregular bone (eg. vertebrae)
What type of ossification does flat bone do for development
Most flat bones develop via intramembranous ossification
- inside a membrane
- Starts out with some kind of membrane
- bone develops in that membrane
Explain the process of Intramembranous Ossification
- Mesenchymal cells in CT membrane or sheet cluster
- Cells differentiate into osteoblasts
- Create an ossification center
- Site where you are making bone
- Osteoblasts secrete osteoid
- Type I collagen and matrix without minerals
- Which then become mineralized
- Osteocyte forms in a lacuna

Explain the slide containing intramembranous ossification

Woven bone (faster)
Newly made
Collagen in multiple directions

What is newly formed bone called?
primary bone or woven bone
NOT LAMELLAR BONE or secondary bone
WOVEN BONE
Collagen in multiple directions, instead of ordered
Because it is faster
- Maturation stage:
- Marrow cavity with blood vessels
-
Immature woven trabeculae
- Collagen fibers oriented randomly
- Mesenchymal cells condense and form the periosteum
-
Remodeling of woven bone >>> Lamellar bone
-
Collagen fibers oriented in parallel
- Formation of cancellous or spongy bone
-
Collagen fibers oriented in parallel

Explain endochondral ossification during fetal development
From cartilage >>>> to bone
DURING FETAL DEVELOPMENT and GROWTH IN LENGTH OF BONE
- Mesenchymal cells condense
- Formation of a chondrocyte (Type II Collagen)
- Hyaline cartilage
- Glassy and do not see fibers
- Forms a perichondrium
- Cartilage deteriorates and turns into bone in the primary ossification center (center long bone)
- Within the primary ossification center)
- Osteoblasts build
- Osteoid and bone is developed (eosinophil)
- Cartilage breaks down (basophilic)
- Initially, form woven bone in the ossification center
- Within the primary ossification center)
SECONDARY OSSIFICATION CENTERS THEN DEVELOP AT THE ENDS OF THE CARTILAGINOUS STRUCTURE
** Woven bone eventually remodels to lamellar bone

Explain how bone grows in width
APPOSITIONAL OR PERIOSTEAL GROWTH
Growth in width or thickening of a bone
- Osteoblast lays down new bone on the surface
- Edge of the bone instead of epiphyseal growth plate

Name and describe the Epiphyseal growth plate zones

-
Zone 1 - Hyaline cartilage
- Resting zone
- Cell type = chondrocytes
-
Zone 2 - Proliferation
- Cells divide
-
Zone 3 - Hypertrophy
- Cells are getting longer
- Compresses the surrounding cartilaginous matrix
-
Zone 4 - Calcification
- Chondrocytes die (apoptosis)
- Because cartilage making is no longer necessary
- Cartilage matrix becomes calcified (more basophilic)
- Chondrocytes die (apoptosis)
-
Zone 5 - Ossification
-
Blood vessels and osteoblasts invade the tissue
- Lays down osteoid
- Creates mineralized bone (eosinophilic)
- Lays down osteoid
-
Blood vessels and osteoblasts invade the tissue

What type of bone will initially be formed at the growth plate?
Woven bone (quick remodeling)
When epiphyseal plate is closed = epiphyseal line and no more cartilage remains in the bone